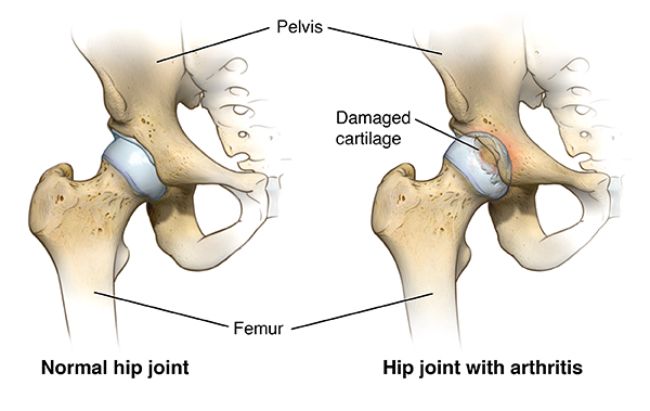
Hip arthritis is a degeneration of the hip joint’s cartilage. The ball of the hip joint is located at the top of the thighbone (the femoral head). Cartilage separates the ball from the socket (the acetabulum). During leg movement, the cartilage serves as a seamless interface between the ball and the socket, facilitating smooth floating and rotation of the ball. Stability is ensured by the labrum, a robust cartilage lining the outer edge of the socket.
Hip cartilage that has been injured becomes tough. As the cartilage thins, the space between the bones diminishes. In severe situations, bone scrapes against bone, making movement painful and stiff. Bone spurs, which are bony outgrowths along the edges of a bone that change its shape, may also form when there is contact between bones at any location.
Overview
What constitutes hip arthritis?
Hip arthritis occurs when the cartilage within the hip joint deteriorates or sustains damage, resulting in the grinding of bone surfaces together, which become rough. This leads to pain and stiffness, impairing leg movement.
Various types of hip arthritis exist, all characterized by a depletion of cartilage within the hip joint, eventually resulting in bone-on-bone contact and joint degradation.
Types of Hip Arthritis
Five primary forms of arthritis can impact the hip joint. They include:
- Osteoarthritis: Osteoarthritis, often termed as “arthritis of the bone,” is the most prevalent type of arthritis. It’s frequently attributed to the wear and tear experienced by joints, which elucidates its higher occurrence among older individuals compared to younger ones. The hip joint consists of the rounded tip of the thigh bone, known as the femoral head, which inserts into the acetabular socket, forming the hip socket.. Within this ball-and-socket joint, a smooth cartilage lining facilitates effortless joint movement. When this cartilage wears down, the remaining rough surfaces of the ball-and-socket rub against each other, resulting in discomfort. Over time, osteoarthritis can lead to joint degeneration or permanent damage.
Osteoarthritis affecting the hip (as well as other body parts) has been associated with the following factors:
- Structural irregularities in the hip joint (such as hip dysplasia, femoroacetabular impingement)
- Increasing age
- Obesity
- Previous hip injuries or trauma.
2. Rheumatoid arthritis: Rheumatoid arthritis is a systemic condition, meaning it affects the entire body rather than just the hip joint. The inflammation is triggered by an immune system response rather than by joint wear and tear.
Similar to other joints in the body, the hip joint is safeguarded by a specialized capsule that envelops it entirely. This capsule features a unique lining known as the synovial lining and is filled with lubricating fluid (joint fluid) to facilitate smooth joint movement. Rheumatoid arthritis commonly leads to swelling of the synovial lining, resulting in pain and swelling. Over time, rheumatoid arthritis can lead to the breakdown of both bone and cartilage within the joint.
3. Ankylosing spondylitis: Ankylosing spondylitis is a persistent inflammation affecting the spine and sacroiliac joint (the connection point between the spine and the pelvis), occasionally extending to involve the hip joint. This condition can manifest in individuals of all age groups, including children, and commonly initiates in individuals aged 17 to 35. It is found more in women.
Individuals with ankylosing spondylitis typically undergo periods of exacerbation, known as flares, during which the condition worsens, followed by phases of remission characterized by mild to no symptoms.
4. Systemic lupus erythematosus: It is commonly known as lupus, is a systemic autoimmune condition capable of affecting various body parts, including the hip joint. When lupus affects the hip, it can lead to inflammation and joint damage. While lupus can develop at any age, it is most frequently observed in women aged 15 to 35.
5. Psoriatic arthritis: Psoriatic arthritis, as implied by its name, is associated with the skin ailment psoriasis. It results in joint discomfort, swelling, and stiffness and can impact any joint, including the hip. Typically, individuals with psoriatic arthritis experience the skin condition initially (characterized by scaly red patches of skin), but it is also feasible to develop psoriatic arthritis before the onset of the skin condition.
Stages of Hip Osteoarthritis:
- Stage 1: Initial wear and tear of the hip joints along with minor bone spur formation, often accompanied by minimal or no pain.
- Stage 2: Onset of cartilage breakdown and visible bone spur growths evident on X-rays. Symptoms include hip pain, discomfort, and stiffness. This stage is alternatively known as early hip osteoarthritis.
- Stage 3: Progression of cartilage erosion and narrowing of the gap between hip bones. Routine activities such as walking, kneeling, or squatting result in pain and swelling. This stage is also known as moderate hip osteoarthritis.
- Stage 4 (the most advanced stage): Nearly complete loss of cartilage leading to chronic inflammation. Pain and stiffness are persistent, affecting daily activities.
Symptoms & Causes
Hip Arthritis Symptoms
Symptoms of hip arthritis, regardless of the specific type of arthritis, may include:
- Hip joint pain, which can extend to the groin, outer thigh, or buttocks.
- Pain typically intensifies in the morning and improves with activity.
- Difficulty walking or a noticeable limp while walking.
- Pain that exacerbates with vigorous or prolonged activity.
- Hip stiffness or limited range of motion.
In individuals with rheumatoid arthritis or lupus, fatigue and weakness may also manifest. Arthritis often manifests in episodes of flares followed by periods of remission, although some individuals may experience a relatively consistent level of pain without flares.
Arthritis can affect more than one joint in the body, so someone with osteoarthritis of the hands might also develop the condition in the hip. Rheumatoid arthritis and lupus typically impact both hips simultaneously, whereas osteoarthritis and psoriatic arthritis may only affect one hip.
Causes:
In individuals with inflammatory arthritis, the immune system fails to regulate itself properly, leading it to attack the body’s own tissues. This immune cell invasion of tissues results in inflammation where it’s unnecessary, and the release of certain chemicals leads to damage to the affected tissues.
While the precise cause of inflammatory arthritis remains unknown, there is evidence suggesting that genetics contributes to the development of certain forms of the disease.
Diagnosis
How is hip arthritis diagnosed?
Your physician may employ the following diagnostic methods to ascertain if you have hip arthritis:
- Review of medical history and physical examination
- Blood tests to detect genetic markers and/or rheumatoid arthritis (RA) antibodies
- X-rays to assess cartilage loss
Cartilage isn’t visible on X-rays, but the space between the bones of the hip joint can be observed. Narrowing of this space may indicate cartilage loss. X-rays also reveal bone spurs and cysts, which develop due to osteoarthritis. Typically, MRI of the hip is unnecessary for diagnosing arthritis.
Treatment
Nonsurgical Treatments for Hip Arthritis
- Adjusting activities may alleviate painful flare-ups. It’s advisable to avoid activities that exacerbate hip arthritis, such as running, jumping, and other high-impact exercises.
- Lifestyle adjustments, including weight loss, can lessen pressure on the hip joint.
- Physical therapy exercises aim to enhance hip strength. Participating in low-impact exercises and activities like swimming and cycling, and maintaining regular physical activity, are crucial for managing hip arthritis symptoms
- Applying heating pads can help alleviate inflammation in the hip.
- Medications and injections, such as corticosteroid injections, hyaluronic acid injections, platelet-rich plasma injections, as well as vitamin and mineral supplements, and immunosuppressive or biologic medications, can aid in managing pain and inflammation. The effectiveness of these medications varies depending on the type of arthritis.
- Walking aids like canes or walkers offer support during walking.
Surgical Treatment
A significant number of individuals with hip arthritis are suitable candidates for surgery. Surgical procedures can alleviate pain, enhance quality of life, and increase mobility, often enabling individuals to carry out daily activities with fewer or no limitations.
- Hip replacement surgery, also known as hip arthroplasty, involves replacing one or both ends of a damaged hip joint with artificial implants.
- Hip fusion, a procedure to fuse the bones of the hip joint, was previously the primary surgical option for hip arthritis before replacement surgeries became prevalent. However, it is now considered a final treatment choice as it significantly restricts mobility.
