Knee Pain After Running: 7 Causes And Treatment Options One Must Know!
What is knee pain after running?
If one experiences knee pain after running, one might worry about it. But don’t panic immediately! Sometimes, feeling sore or achy during or after exercising isn’t a big deal. It could just be your body’s way of saying it’s been working hard. Runner’s knee, also called Patellofemoral Pain Syndrome, is when you feel a dull pain around the front of your knee, where it meets your thigh bone. This is common among people who run or jump a lot, there is a knee pain. It can happen in one or both knees and affects both kids and grown-ups. If you want to know more about the signs of a runner’s knee and how to deal with knee pain after running, keep reading!
body’s way of saying it’s been working hard. Runner’s knee, also called Patellofemoral Pain Syndrome, is when you feel a dull pain around the front of your knee, where it meets your thigh bone. This is common among people who run or jump a lot, there is a knee pain. It can happen in one or both knees and affects both kids and grown-ups. If you want to know more about the signs of a runner’s knee and how to deal with knee pain after running, keep reading!
Common Knee Injuries caused by knee pain after Running:
- Runner’s Knee
- IT Band Syndrome
- Patellar Tendonitis
- Arthritis
- ACL Injuries
- PCL Injuries
Let us see the causes, symptoms & treatment of knee injuries, caused because of knee pain after running
1. Runner’s knee
Running puts a lot of stress on your joints because you’re hitting the ground hard over and over again. This can lead to a condition called “Patellofemoral Pain Syndrome” (PFPS), also known as runner’s knee. It causes pain in the front of your knee or around your kneecap. This pain is often caused by doing the same movements over and over, having weak or tight leg muscles that make your kneecap misaligned, and sometimes, by not running with the right form.
Symptoms
Dr. Preetesh Choudhary says that if you have a runner’s knee, you’ll usually feel pain under or at the front of your kneecap when you run. Other symptoms include:
- Pain when you bend your knee during activities like climbing stairs or hiking.
- knee pain, especially in front of knee.
- A popping or crackling sound when you bend your knee
Treatment
Runner’s knee often happens because you’ve been using your knee too much. So, it’s important to give it a break for about two weeks. After that, try running on softer surfaces like grass or sand, and put ice on your knee after each run to help it heal. If the pain keeps coming back, it might be a good idea to see a physical therapist to work on any weak muscles, especially around your hips.
At home, you can use the RICE method—rest, ice, compression, elevation—to ease the pain of the runner’s knee. You can also take over-the-counter anti-inflammatory drugs if your doctor says they’re safe for you.
Prevention
To avoid it, make sure you increase gradually how much you run, as advised by Dr. Preetesh. Also, as doctors suggest doing other types of exercise alongside running, like stretching and resistance training, to keep your muscles strong and balanced.
2. IT Band Syndrome (ITBS)
Your Iliotibial (IT) band is like a strong rope that links your knee and hip together, helping to keep your knee steady.
When you use it too much or put too much strain on it, you can get IT band syndrome (ITBS). This happens when your IT band gets tight, irritated, and swollen. The main sign is feeling pain on the side of your knee.
Types of ITBS:
There are two types of iliotibial band syndrome: one-sided (in one leg) and both-sided (in both legs). When it affects both legs, it’s known as Bilateral Iliotibial Band Syndrome.
Symptoms
When your iliotibial band is tight, it can cause several symptoms:
- Hip pain: The band rubs against a bony part in your hip, leading to inflammation and pain. Sometimes, you may hear a snapping sound.
- Clicking sensations: You might feel a snap, pop, or click on the outer side of your knee.
- Knee pain: The tight band rubs against the outer part of your knee, causing inflammation and pain.
- Warmth and redness: The outside of your knee may look discolored and feel warm to touch.
Initially, the pain may only occur after exercising. However, as the syndrome progresses, you may feel it throughout your exercise routine and even during rest.
Diagnosis of Knee Pain
Here are some steps you can take:
- Touch the outer part of your knee to check if that’s where your iliotibial band syndrome pain is coming from.
- Try moving your hip away from your body while holding your knee. If you feel pain and can’t move your hip much, it might indicate a problem.
- Move your knee in different directions to see if it causes any knee pain.
To make sure you have iliotibial band syndrome, your doctor might also order some imaging tests such as:
- MRI- The MRI can help your doctor rule out other injuries such as a meniscal tear or a lateral collateral ligament (LCL) injury, narrowing down the possibilities to find the cause of your symptoms.
- Ultrasound
Treatment
There are various treatments available for iliotibial band syndrome, some of which you can do at home, while others require help from a healthcare provider. Here are the common treatments:
- Rest: It’s often advised to avoid exercising the affected leg until the pain goes away and the syndrome heals. Doctors here at MLs Clinic can guide you on how much rest and activity you need.
- Pain medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) can help relieve pain. Make sure to visit us at MLs Clinic for the right dosage.
- Physical therapy: Physical therapists can guide you through stretches, strengthening exercises, and other treatments to alleviate hip and knee pain. These therapies can help loosen your iliotibial band and reduce tension. They can also advise you on proper warm-up and cool-down routines before and after exercise. A physical therapist may teach you how to use a foam roller to massage your body and ease tension.
- Posture training: Your body posture during daily activities and sports can affect iliotibial band syndrome. Learning proper posture techniques can help manage the condition.
- Steroid injections: As recommended.
- Surgery: Surgery for iliotibial band syndrome is uncommon and usually considered when other treatments like medications and physical therapy haven’t been effective. Your doctor will discuss this option with you if necessary.
Always consult with your trusted nearest Orthopedic Surgeon before starting any treatment to ensure it’s suitable for your condition and health status.
Prevention
How can I lower my chances of getting iliotibial band syndrome (ITBS)?
Preventing ITBS can be tough, especially for athletes like skiers, cyclists, or long-distance runners. However, you can try changing how you do these activities to reduce your risk. Here are some examples:
- Avoid running on steep hills or slanted surfaces.
- Make sure you use the right technique for any activity you do.
- Gradually increase the intensity of your training, instead of suddenly speeding up while cycling, slowly build up your pace.
- Take your time to warm up before exercise and cool down afterward.
- Wear shoes that provide good support for your feet.
3. Patellar Tendonitis
Patellar tendonitis occurs when the tissue of the patellar tendon becomes swollen or irritated due to overuse. This knee injury is common among athletes who are highly active.
The pain from patellar tendonitis can range from mild to severe and tends to get worse over time. If not treated, the pain and discomfort can become severe, affecting your ability to perform activities. It may even prevent you from participating in sports or other activities altogether.
Symptoms
Symptoms of patellar tendinitis can include:
- Pain or dull ache right under the kneecap (knee pain), at the top of the shinbone.
- Feeling stiff, which might make it difficult to fully straighten your knee.
- Pain gets worse with specific movements, like squatting or walking downstairs.
Diagnosis & Tests of Knee Pain:
Diagnosis
We at MLs Clinic, will do a physical exam to check your symptoms. They might press on different parts of your knee’s patellar tendon to see where it hurts. They’ll also gently move your knee in different ways to see how well it can move.
Tests
- X-Ray of Knee,
- Ultrasound & MRI- In more serious or long-lasting cases of patellar tendonitis, both ultrasound and MRI scans can detect any damage to the structure of the patellar tendon.
Treatment of Knee Pain:
Here are some things you can do to help with patellar tendonitis:
- Take it easy: Avoid activities or movements that make your symptoms worse. Pushing through the pain could make the tendon tissues more damaged.
- Rest: Try to stay off your feet as much as possible. Resting gives your body time to heal.
- Apply ice: If your knee is swollen, applying an ice pack to the area for 15 minutes at a time, a few times a day, might help reduce swelling.
- Take pain relievers: Over-the-counter anti-inflammatory medicines can help with minor aches or knee pains.
- Support your knee: Knee Replacement Surgeon might suggest wearing a knee brace or other support device to help ease the pain.
- Try physical therapy: A trained therapist can teach you special exercises and stretches to gradually strengthen and stretch the injured tendon tissues. Physical therapy might also help reduce your discomfort.
- Consider surgery: Surgery for patellar tendonitis is not common. But if imaging tests show a tear in the tendon, your Orthopedic Doctor might recommend surgery to repair the damaged tissues.
Arthritis
Arthritis is a condition that harms your joints, which are where two bones meet in your body. 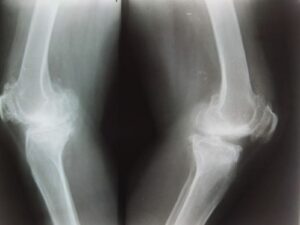
As you grow older, some joints naturally become worn out. Many people develop arthritis because of this usual wear and tear over their lifetime. Arthritis can also occur after injuries that harm a joint or due to certain health issues.
Arthritis can affect any joint, but it’s most common in:
- Hand and wrist
- Knee
- Hip
- Feet and ankle
- Shoulder
- Lower back (lumbar spine)
Types of Arthritis
There are different kinds of arthritis:
- Inflammatory arthritis
- Degenerative or mechanical arthritis
- Connective tissue disease (CTD)
- Infectious arthritis
- Metabolic arthritis
- Childhood arthritis
- Septic arthritis
Symptoms
Arthritis often makes your joints hurt and feel stiff, like you can’t move them well. They might get swollen, change color, or feel tender when you touch them. Sometimes, they even feel warm. Where you feel these symptoms depends on which kind of arthritis you have and which joints it affects.
Certain things can make you more likely to get arthritis. These include:
- Using tobacco: Smoking or using other tobacco products raises your chances.
- Knee Pain
- Family history: If your family members have arthritis, you’re more likely to get it too.
- Activity level: Not being very active can increase your risk.
- Other health issues: Conditions like autoimmune diseases, obesity, or anything affecting your joints can up your chances of getting arthritis.
Diagnosis
Orthopedic Doctor might use special tests to take pictures of your joints, such as:
- X- Ray
- Ultrasound
- Magnetic Resonance Imaging MRI
Treatment
There’s no cure for arthritis, but your doctor will help you find treatments to manage your symptoms. The treatments you need depend on what’s causing your arthritis, which type you have, and which joints are affected.
Common treatments for arthritis include:
- Over-the-counter (OTC) anti-inflammatory medicines.
- Prescription anti-inflammatory medicines.
- Disease-modifying antirheumatic drugs (DMARDs) if you have rheumatoid or psoriatic arthritis.
- Physical therapy or occupational therapy to help you get stronger, move better, and feel more confident.
- Surgery, but usually only if other treatments don’t work.
Surgical Treatment
For arthritis, surgeries can include:
- Synovectomy
- Total joint replacement (TJR)
- Osteotomy
- Joint fusion
5. ACL Injuries
ACL (Anterior Cruciate Ligament) injuries occur when the ligament connecting the thigh bone to the shin bone tears or stretches, often due to sudden stops, changes in direction, or direct impact. These injuries are common in sports like soccer and basketball, causing instability and knee pain.
6. PCL Injuries
PCL (Posterior Cruciate Ligament) injuries happen when the ligament connecting the thigh bone to the shin bone tears or stretches, often due to direct impact to the front of the knee or hyperextension. Less common than ACL injuries, they can cause instability and knee pain, especially during activities requiring pivoting or bending.
7. Meniscal Tear
A meniscus tear happens when the soft cushion in your knee joint gets torn, which can make the inside of your knee pain and hurt. It usually occurs when you twist your knee while your foot is on the ground. It can also happen if you get hit in sports or as you get older and your knee wears down slowly.








Nec ut tellus ornare, orci tortor suspendisse aliquet sollicitudin rhoncus, maecenas suscipit cras porttitor vestibulum vivamus.
Neque turpis vitae eros praesent varius. Egestas pellentesque urna blandit, sed ac leo ut mi, nam wisi, laborum donec erat amet.
Massa suspendisse lorem turpis ac. Pellentesque volutpat faucibus pellentesque velit in, leo odio molestie, magnis vitae condimentum.
Aute mi ut suspendisse velit leo, vel risus ac. Amet dui dignissim fermentum malesuada auctor volutpat, vestibulum ipsum nulla.
Comments are closed.