Brief of Shoulder Replacement Surgery
A smooth, pain-free range of motion is made possible by the cartilage that lines the shoulder joint and helps to protect the bones. When cartilage starts to degrade due to regular wear and strain, shoulder arthritis can be a crippling condition. Osteoarthritis is a degenerative disorder that frequently affects older people and is characterized by inflammation, swelling, and chronic shoulder pain. Individuals who have attempted non-surgical interventions like arthroscopic shoulder surgery, physical therapy, medications, and injections without relief from painful arthritis symptoms may qualify as candidates for shoulder replacement. Shoulder replacement surgery, also referred to as shoulder arthroplasty, enables patients to resume a healthy, regular life after the procedure.
What is Shoulder Replacement Surgery?
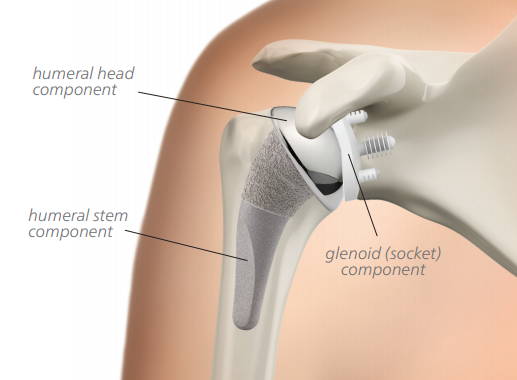
Shoulder replacement surgery involves removing the damaged sections of the shoulder and substituting them with artificial components known as a prosthesis. There are two options for treatment: either replacing just the head of the humerus bone, which is called the ball, or replacing both the ball and the socket, known as the glenoid.
What medical issues does shoulder replacement surgery address?
Shoulder replacement surgery addresses various conditions, primarily shoulder arthritis and severe fractures. Arthritis affecting the shoulder typically falls into two categories: osteoarthritis and inflammatory arthritis.
- Osteoarthritis results from the gradual deterioration of cartilage within the joint due to prolonged use. While this condition commonly affects other joints like the knees, hips, or fingers in older adults, it can also occur in exceptionally active individuals, such as athletes who subject their shoulders to constant strain. Sometimes, severe acute injuries, like a torn rotator cuff or shoulder fracture, contribute to this long-term damage.
- Inflammatory arthritis encompasses several chronic autoimmune diseases without a fully understood cause. Rheumatoid arthritis and ankylosing spondylitis are two types that specifically affect the shoulder. Many patients with these conditions experience reduced pain and improved shoulder function following replacement surgery. Additionally, some ankylosing spondylitis patients may benefit from elbow replacement procedures.
What are its Symptoms?
Shoulder replacement surgery is recommended for patients experiencing joint dysfunction, typically due to conditions like osteoarthritis, rotator cuff tear arthropathy, avascular necrosis, rheumatoid arthritis, or in rare cases, severe fractures from trauma. Usually, other treatment options such as physical therapy and medications are explored first. You might be considered for shoulder replacement surgery if you:
- Experience severe shoulder pain that hampers daily activities like bathing, dressing, or reaching.
- Have limited shoulder motion.
- Exhibit shoulder weakness.
- Endure such intense pain that it disrupts your sleep.
- Have tried anti-inflammatory drugs, cortisone injections, and physical therapy without relief.
- Have undergone prior arthroscopic surgery, rotator cuff repair, or fracture repair that didn’t alleviate symptoms.
What occurs during the initial appointment for shoulder replacement surgery?
During your first consultation with the orthopedic surgeon, several steps are taken. This includes a series of x-rays, a physical examination, and a comprehensive review of your medical history.
- The physical examination aids the surgeon in identifying the source of pain and assessing any decrease in range of motion.
- X-rays help reveal bone spurs, damaged joint surfaces, and any narrowed joint spaces. In cases of shoulder trauma or injury, x-rays assist in determining whether a fracture can be treated or if shoulder replacement is necessary.
- Providing a detailed history of your shoulder problem involves describing the level of pain during activity, restricted use, loss of motion, and pain while at rest. Additionally, prior treatments such as medications, injections, physical therapy, and previous surgeries are discussed.
Based on this information, you, your family, and the orthopedic surgeon collaborate to determine the most suitable next steps.
Who is not suitable for shoulder replacement surgery? 
Certain individuals are not ideal candidates for shoulder replacement surgery. These include those who:
- Experience symptoms that are not notably impairing.
- Experience loss or paralysis of both the rotator cuff and deltoid muscles.
- Have active infections.
- Have a progressive nervous system disease that affects the joint (evaluated case by case).
Additionally, some patients in the early stages of osteoarthritis may opt to initially pursue nonsurgical, conservative management options to assess whether shoulder replacement is necessary or can be postponed. These measures may involve:
- Physical therapy.
- NSAIDs (nonsteroidal anti-inflammatory drugs).
- Corticosteroid injections.
What other choices are there instead of shoulder replacement?
Shoulder arthroscopy is often suggested for individuals with shoulder conditions affecting the surrounding ligaments, muscles, and tendons, like a rotator cuff injury or torn shoulder labrum. Arthroscopy, a minimally invasive surgical procedure, is one of the most common types of shoulder surgery. However, it mainly addresses conditions leading to arthritis rather than arthritis itself. This option is typically beneficial for patients who haven’t progressed to bone-on-bone arthritis yet.
General Instructions:
- Follow your healthcare provider’s instructions for driving. Arrange for a ride home upon discharge.
- Avoid lifting anything heavier than a glass of water for the first two to four weeks.
- Refrain from lifting heavy objects for two months.
- Gradually resume arm movement within the limits of pain.
- Continue prescribed exercises at home under the guidance of your physical therapist and healthcare team.
- Be cautious not to overexert yourself.
- Refrain from using your operative arm to push yourself up from a bed or chair.
- Avoid repetitive heavy lifting and refrain from participating in contact sports.
- For the first six weeks after surgery, avoid placing your arm in extreme positions, such as stretching it straight out to the side or behind your back.
Recovery and Follow-Up Guidelines:
Home Care Instructions:
- Monitor the incision daily for increased swelling or drainage.
- Keep the dressing intact. It is waterproof, allowing you to bathe and shower. Let water run over it and pat it dry afterward. The dressing will be removed at your first follow-up appointment.
- Upon discharge, you will receive a return appointment 10 to 14 days later to remove the dressing and a prescription for pain medication.
- Your healthcare provider will inform you of specific precautions and activity limitations.
Post-Discharge:
Your rehabilitation will continue progressively. Achieving optimal benefits may take between six months to one year. It’s important to understand that progress can be slow and may not always be consistent. You must remain committed to your therapy program, performing exercises several times a day for five to 10 minutes each session. During the first month after surgery, avoid lifting anything heavier than five pounds and refrain from using your arm to lift, reach, push, or pull above waist level for six weeks.
